Issue 12 | October 2025


Hello
And welcome.
Dave Middleton, Executive Chair, amii
Welcome to the latest amii members’ newsletter.
I trust this finds you well and that your business continues to thrive as we approach the close of another year for our industry.
In this edition, we turn our attention to some of the most significant developments shaping health and protection today. Professor Gordon Wishart of Check4Cancer opens with a compelling exploration of how early detection not only saves lives but also delivers measurable returns for employers, insurers, and intermediaries alike. We are also joined by Kelly McCabe, Co-Founder and CEO of Perci Health, who introduces the concept of Performance Oncology—a bold, evidence-based model transforming cancer recovery and survivorship for working-age adults.
Our feature from UKGI provides timely insight into the fast-evolving world of Artificial Intelligence, offering practical “Ground Rules” to help firms navigate regulatory expectations and harness AI responsibly across their operations.
Finally we are delighted to welcome Denis Global as a new corporate member of amii. With more than 25 years of international experience in insurance systems, automation, and TPA services, Denis Global brings valuable expertise in innovation, compliance, and operational excellence to our growing community. the UK and beyond. Mark Till CEO, of Unum UK shares the rationale for why they entered the Cash Plan market with the launch of Health Plan 360.
If you haven’t already done so please sign up and join us at the Autumn Summit on 13th November at One Great George Street, London. This year’s event features keynote speaker Dr Samantha Hiew, founder of ADHD Girls, Liam Kennedy of Vitality (and of course amii), Ian Forrester of Cubic Garden, Dr Roshane Mohidin of Aviva and Dr Rebecca Mansfield of Unum, Jill Hambley and Isabella Macfarlane ACII of Insurance Compliance Services Ltd, a UKGI Compliance business, in addition to expert cancer panellists Professor Ben Kelly of Reframe Cancer and Kelly McCabe of Perci Health. Alongside plenty of opportunities to connect and network with peers.
As ever, thank you for your continued engagement and support. We look forward to seeing many of you in London next month.
Newsletter Contents.

Creating Healthy Business
Through Early Cancer Detection.
Professor Gordon Wishart, Chief Medical Officer, Check4Cancer
Cancer remains the leading cause of death in the UK, responsible for 26% of all deaths – that’s over 460 lives lost every day. Despite remarkable advances in treatment, the UK still lags behind other countries in survival rates. The reason? Too many cancers are diagnosed late, when symptoms are advanced, treatments are more complex and expensive, and outcomes are poorer.
As professionals shaping corporate health strategies, you already know how important private medical insurance (PMI) and wellbeing programs are for supporting employee health. But here’s the big question: how can we tackle the single greatest health risk – cancer – while also managing its impact on business costs?
The answer lies in a targeted, specialist approach to early cancer detection. This isn’t about general wellness initiatives; it’s about clinical precision, evidence-based strategies, and measurable outcomes.

A decade dedicated to early detection
In a marketplace saturated with broad-brush wellbeing platforms, Check4Cancer stands out as the UK’s only dedicated specialist in early cancer detection. For over a decade, we’ve focused exclusively on this critical area, refining our expertise and services to deliver unparalleled clinical governance and measurable results.
This singular focus makes a difference. While general health providers offer a wide range of services, they often lack the depth of expertise needed for early cancer detection. At Check4Cancer, every pathway, algorithm, and diagnostic tool is designed with one goal: to catch cancer early, when it’s most treatable. This dedication ensures our services are backed by evidence, guided by leading UK cancer specialists, and continuously improved.
Our numbers tell a compelling story. With over 260,000 services delivered, we’ve built one of the largest private datasets in early cancer detection. We focus on six of the most common cancers-breast, bowel, cervical, lung, prostate, and skin- with evidence consistently showing that detecting cancer early saves lives, reduces anxiety, and lowers costs.
Independent audits demonstrate clear improvements over national averages. In our breast diagnostic pathway, 92% of cancers were detected at stage 1 or 2, compared with 83% through the NHS two-week urgent referral route. In our national teledermatology service, 96% of melanomas detected were early stage, well above the 85% national benchmark.
These aren’t abstract statistics: they represent hundreds of people whose cancers were found early enough to be treated effectively, returning them to health – and work – sooner. For insurers and employers, that translates directly into measurable cost and productivity benefits.
Employers are increasingly recognising the value of cancer prevention and early detection as part of their workplace wellbeing strategies. In fact, research shows that cancer screening is one of the most valued employee benefits.
At Check4Cancer, we make it easy for businesses of all sizes to offer these life-saving services:
- Education: Webinars, campaigns, and awareness initiatives to help employees understand cancer risks and the importance of early action.
- MyCancerRisk©: A digital tool that assesses an employee’s risk for six common cancers and directs those at higher risk to funded screening. Trusted by companies like M&S and Microsoft, this program has already supported over 35,000 individuals.
- Flexible Benefits: Cancer screening as an optional benefit within existing wellbeing platforms.
- Bespoke Campaigns: Tailored screening initiatives designed around workforce demographics and risk profiles, from senior leadership programs to nationwide rollouts.
Our Cancer Impact Calculator© helps employers and intermediaries estimate the return on investment (ROI) from cancer screening. It also highlights which cancers to prioritise based on workforce data, enabling businesses to plan future health campaigns based on objective evidence.

Measuring What Matters: Health ROI and Human Value
Early cancer detection isn’t just about saving lives-it’s also about creating healthier, more productive workplaces. Here’s how it benefits businesses:
- Boosts employee wellbeing: Offering early detection services shows employees you genuinely care about their health.
- Reduces costs: Late-stage cancer treatment is far more expensive. Catching cancer early helps insurers and employers manage these costs.
- Delivers measurable ROI: We provide data and reporting to help intermediaries demonstrate the value of our programs, strengthening client relationships with tangible results.
With over a decade of experience, more than 260,000 services delivered, and a commitment to clinical excellence, Check4Cancer is the trusted partner for tackling this critical health risk.
Our high patient satisfaction rating (4.84/5 on Doctify), partnerships with leading UK consultants, and Clinical Advisory Board are just a few of the reasons why insurers and intermediaries trust us. We don’t replace existing PMI frameworks-we enhance them, offering a complementary, data-driven solution that adds value for you and your clients.
Our focus remains on three priorities: maintaining clinical excellence, expanding digital access, and deepening collaboration across the health insurance community. The burden of cancer will continue to grow, but the opportunity to change outcomes has never been greater.
By combining data, technology, and clinical expertise, we can shift cancer from being a catastrophic health event to a manageable, predictable risk.
Early detection is not just good medicine – it’s good business.
Have you registered to join the for Members Only section of our website?
The for Members Only section of our site provides a wealth of content for members, as well as access to all the benefits that being a member of amii provides. If you haven’t done so already, please do register to take advantage of everything your membership offers. You can do so by following the link below.

Meet new amii corporate member Denis Global.
The company specialises in delivering dynamic third-party administration (TPA) solutions through both its proprietary Software-as-a-Service (SaaS) platform and as an outsourced services provider. Denis Global’s user-friendly optimisation tools have been developed and refined over many years of research and testing. Their offering ranges from claims services to customer fulfilment, from policy management to premium collection – helping partners achieve operational excellence across the insurance lifecycle.
The business is led by a team of international industry experts with wide-ranging experience in IT development, underwriting, claims, employee benefits management, administration, compliance, and product innovation.
Today, Denis Global’s systems and software power organisations of all sizes across multiple markets worldwide. Their clients include insurers, MGAs, brokers, underwriters, employee benefits providers, HR departments, and financial services firms.
Whether organisations require support in a specific area of insurance administration or a full-stack solution for back-office management, Denis Global provides scalable systems designed to improve efficiency, enhance service delivery, and strengthen competitive positioning. As Director Scott Roberts of Denis UK explains:
“At Denis Global, our goal is to empower insurers, MGAs, brokers, and insurance providers with flexible, DORA-compliant systems and integrations that grow with their business.
“Joining amii aligns with our commitment to supporting innovation, collaboration, and continuous improvement across the health and protection insurance landscape. We’re looking forward to contributing to the conversation, learning from peers, and supporting a community that’s helping raise standards in this space.”
Denis Global’s configurable rules engines and algorithms enable accurate, efficient automation of high-volume claims across all classes of personal insurance.
In addition to standard non-clinical rules (such as financial, quantity, and time-limit checks), Denis Global systems incorporate configurable clinical rules for relevant products, including dental and optical. This ensures that claims handling is both precise and appropriate for each line of business.
Denis UK provides outsourced claims handling, or brokers can integrate Denis Global’s rules-based system into their own operations. This powers in-house processing with smart automation, integrated translation tools, automated customer communications, and optional call-centre support. White-labelled online portals and claim-and-pay functionality enable straight-through claims processing across multiple product lines.
Denis Europe, meanwhile, has a strong focus on dental claims handling. Its advanced software applies both clinical and financial rules to each case, enabling rapid processing and fraud detection. Solutions include membership management, end-to-end claims handling, float management and reconciliation, secure web submission portals, and multilingual customer service. The offering also extends to product design and customer service support for dental insurers.
By applying clinical intelligence and advanced automation, Denis Global makes it possible to streamline even the most complex and high-volume claims environments.
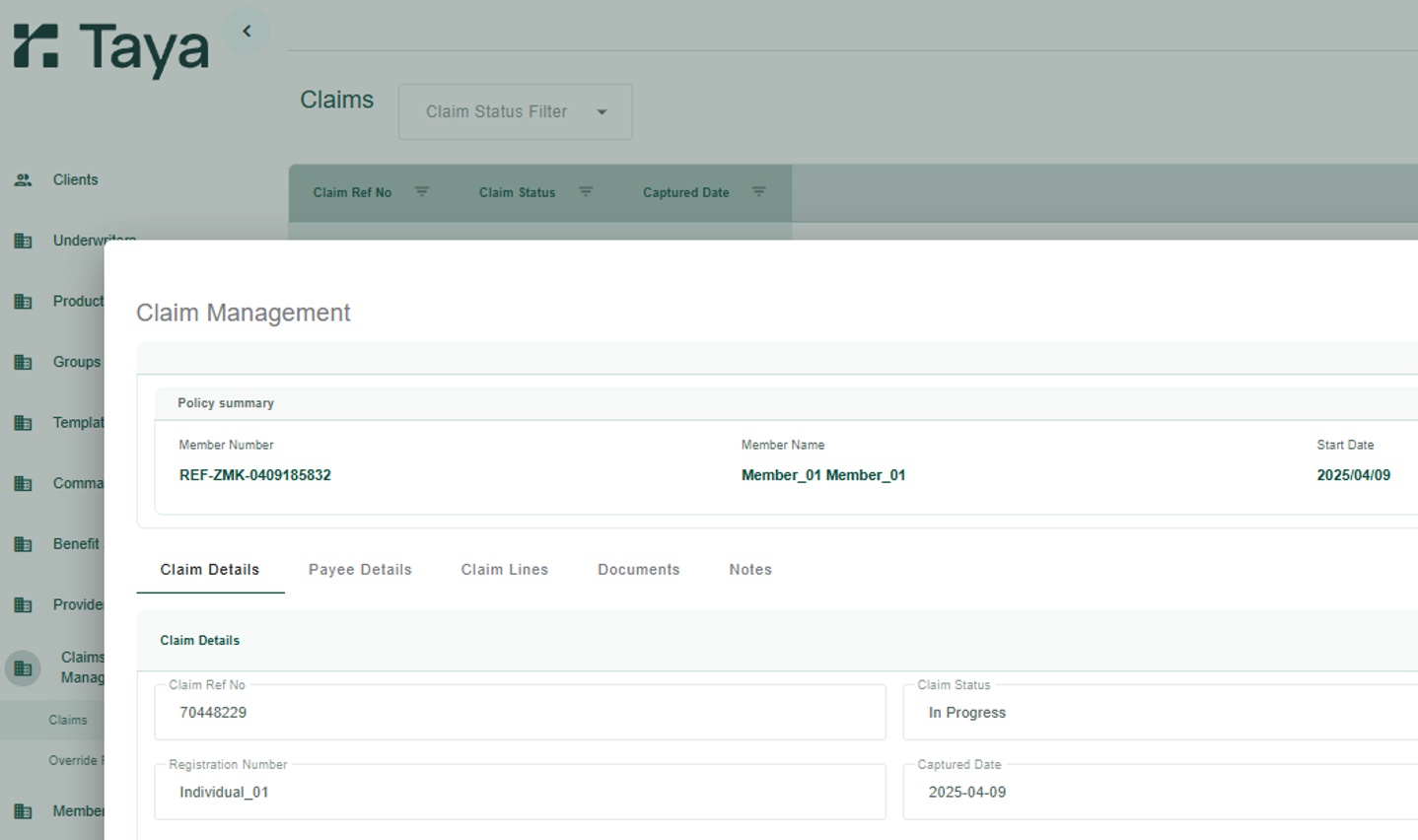
At the centre of Denis Global’s proposition is Taya, the company’s proprietary cloud-based SaaS platform. Taya is a no-code, globally accessible solution that can be configured to meet the precise requirements of any insurance business.
The platform allows organisations to choose the level of functionality and support that fits their needs, with frictionless integration into existing systems. Key features include:
- Rapid configuration of benefit levels
- Accurate pricing driven by data insights
- Multi-channel distribution (direct or via API integration)
- Automated billing, collections, commission calculations, and reconciliation
- End-to-end integration with policy administration and invoicing tools
- Streamlined processes across the entire policy lifecycle
- Optimised claims handling with built-in automation
By combining flexibility with resilience, Taya enables insurers, brokers, and MGAs to operate with confidence in any regulatory landscape.
A key differentiator for Denis Global is its innovative use of artificial intelligence to support modular insurance solutions development. Our systems are developed within a controlled, highly secure offline environment, ensuring that proprietary code and intellectual property remain protected during the build process.
The machines use artificial intelligence to learn from our systems and write new and additional code. Meaning AI is embedded not just as a support tool, but as a developer in its own right – effectively building and refining Denis Global’s software autonomously.
In practice, this allows us to rapidly produce customised prototyes – such as broker portals and client-specific tools – tailored precisely to partner requirements. The result is a secure, efficient, and highly adaptable development process without risk of intellectual property leakage. Working prototypes can rapidly be coded and added to a live environment.
By combining stringent security, modular system architecture, and AI-driven automation, Denis Global enables brokers and insurers to create business solutions in a fraction of the time it would traditionally take.
As amii’s newest corporate member, Denis Global looks forward to collaborating with intermediaries, MGAs, and insurers to raise service standards across the health and protection sector – supporting innovation, improving operational efficiency, and ultimately helping members deliver better outcomes for their customers.
We’d love to talk about your current insurance business processes, and discuss how we could integrate with your existing offering to help transform your business – whatever its size. Please contact the team on enquiries@denisglobal.com.

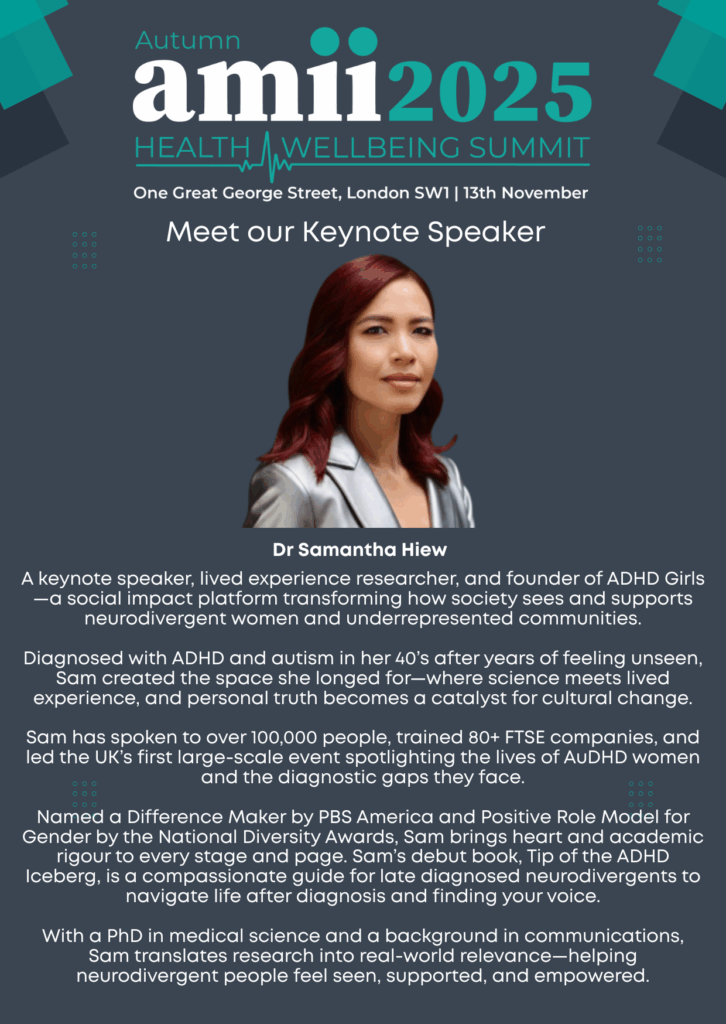
Join us at the Autumn Summit.
This year’s event brings together leaders, innovators, and professionals from across the health and wellbeing sector to share insights, spark new ideas, and explore strategies to drive business growth.
The summit runs from 09:00 to 16:00, followed by a drinks reception from 16:00 to 17:00, providing the perfect opportunity to connect with colleagues and peers in a relaxed setting.
We are delighted to have Dr Samantha Hiew join us. A keynote speaker, lived experience researcher, and founder of ADHD Girls — a social impact platform transforming how society sees and supports neurodivergent women and underrepresented communities.
So, don’t miss this chance to gain valuable knowledge, discover emerging trends, and be part of the conversation shaping the future of health and wellbeing. You can sign up below

Closing the Cancer Care Gap
With ‘Performance Oncology’.
Kelly McCabe, Co-Founder & CEO, Perci Health
When I started my career nearly 20 years ago as an oncology dietitian in the NHS, I was supporting people with head and neck cancer through some of the toughest treatments imaginable. Later, I led a network of private cancer centres and was privileged to work with the clinicians introducing cutting-edge therapies like CAR-T in the UK, treatments that radically improved survival for certain blood cancers and signalled the start of a new era of oncology innovation.
Yet no matter where I worked, whether in the NHS or private care, I saw wide variation in access to care and levels of support. These inconsistencies translate into growing inequalities in cancer outcomes across the country.
The gaps start early: many people are diagnosed late because of missed screening opportunities, or delays in recognising symptoms. During treatment, support is fragmented, with variable access to psychological care, dietetics, physiotherapy, or fertility counselling and once active treatment ends, care stops. In clinic, again and again, I saw people discharged back to their GP after months of gruelling treatment. They were told: “Everything has gone really well, see you in six or twelve months.” Months later, many returned with unmanaged side effects, uncoordinated care, and overwhelming fear of recurrence.
The reality is this: while modern medicine has transformed survival, we have failed to transform recovery. That realisation is why, in 2020, together with my co-founder Morgan Fitzsimons and a group of leading oncologists and cancer surgeons, I launched Perci Health.

Cancer now touches almost every family in the UK, with one in two of us facing a diagnosis in our lifetime. Survival is improving: almost 3.5 million people are living with cancer today, projected to reach 4 million by 2030 and over 5 million by 2040. The fastest growth is among younger adults, between 1995 and 2019, incidence in under-50s rose 24%, compared with 13% across all ages. With retirement ages rising, 36% of diagnoses now occur in working-age people. Cancer is no longer an issue confined to older age. The economic toll is vast, costing the NHS around £15 billion annually, with lost productivity adding at least another £8 billion.
Just as sports medicine brings together specialists to help athletes recover faster and perform at their best, Performance Oncology applies the same principle to people affected by cancer. It’s a proactive, evidence-based model that integrates cancer nurse navigation, remote monitoring, exercise prescription, prehabilitation and rehabilitation, psychological and financial support, return-to-work planning, and multidisciplinary side-effect management. These are all evidence-based interventions, proven to work but difficult to access. When delivered digitally and layered alongside core cancer treatment, these interventions create an accumulative effect — each reinforcing the other to improve treatment tolerance, accelerate recovery, and enhance long-term outcomes.
Through our virtual clinic, members access the UK’s largest community of multidisciplinary cancer specialists, nurses, dietitians, psychologists, genetic counsellors, physiotherapists and more, all coordinated by a named nurse and accessible from home or work.
Technology underpins everything we do. Our API-first platform makes it simple for insurers to integrate us into their digital front doors. It captures structured data across the cancer journey: treatment tolerance, symptom burden, lifestyle risk factors, quality-of-life measures and more.
Our risk-stratified adaptive care model allows us to deliver the right intensity of support at the right time: proactive when risks first emerge, predictive when the data shows someone may be about to struggle, and always personal. For insurers, this ensures resources are directed efficiently; for members, it means care that feels one step ahead.
Morgan’s expertise in digital transformation at leading consumer brands ensures the Perci experience doesn’t feel like traditional healthcare. It feels intuitive, supportive, and designed for the way people actually live and work. That combination, deep clinical expertise with consumer-grade design, is what makes our model unique.
We’re proud to be the only cancer clinic endorsed by Macmillan Cancer Support, who also invested in our most recent funding round. This partnership goes beyond endorsement: it reflects a shared commitment to tackling some of the most urgent challenges in cancer care today.
Together, we are innovating to address new systemic problems that sit outside of hospital walls but directly affect outcomes, from widespread cancer misinformation online, to low health literacy and delayed help-seeking. Shockingly, up to 83% of cancer patients report being exposed to misinformation about treatment, while 43% of UK adults struggle to understand health information that includes numbers.
That’s why we created Perci Guide, a digital, low-cost, scalable tool to cut through misinformation and build cancer literacy across the workforce. It provides employees with trusted, evidence-based resources and on-demand nurse chat, ensuring that no one is left trying to navigate uncertainty alone.
The impact is powerful: when people are better informed, they act earlier, access the right care sooner, and avoid the devastating consequences of delayed diagnosis, with benefits felt by individuals, families, employers, and insurers alike.

We’re just at the beginning. Later this year, following CQC registration, we will launch specialist clinics for complex, underserved cancer side effects: pain, chemotherapy-induced peripheral neuropathy, lymphoedema, and treatment-induced menopause. These issues often prevent people returning to work, and we are determined to change that.
Looking ahead, cancer survivorship will be one of the most important areas of focus in healthcare. With incidence rising among working-age adults and more people living with cancer than ever before, individuals increasingly want support that goes beyond treatment, care that helps them feel well, return to the life they value, and move forward with confidence.
At Perci Health, we’re building a new standard of care, one where surviving cancer means living well, working well, and feeling supported every step of the way. Our pioneering model, Performance Oncology, is something every person impacted by cancer deserves.
For insurers and intermediaries, this is an opportunity to be at the forefront of a profound shift, closing the cancer care gap, improving outcomes, and delivering measurable value for the health and protection ecosystem.

The
AI Ground Rules.
UKGI
Artificial Intelligence (AI) is now everywhere; it is becoming increasingly relevant and even if you are not actively using it, an awareness of its capabilities and pitfalls is vital. Like Amazon’s Alexa but in a more exaggerated way, AI is gradually becoming part of everyday life. However, just as with Alexa, the need for caution and scepticism remains, and rightly so. AI however is capable of a lot more than Alexa (sorry, Alexa!).
AI is evolving rapidly. We feel this next stage mirrors the early days of the internet but at a much faster pace. Back then, we endured slow connections, had to negotiate family phone use for MSN Messenger, and listened to the dial-up tones, with slow and steady progress. Today AI evolves at a lightning speed, on a scale of months, or even weeks.
Recently, the FCA published “AI and the FCA: our approach”. The regulator made it clear that it does not intend to introduce a separate set of rules for AI. Instead, it expects firms to manage AI within the framework of existing regulation. For example, the FCA highlighted how the Consumer Duty, and its rules on accountability and governance under SMCR, already set expectations for how firms should approach the use of AI.
The FCA also referred back to its 2024 publication, AI update, which mapped its existing rulebook against the Government’s guidance on AI.
Of course, turning this into day-to-day practice is not always straightforward. With that in mind, the following ‘Ground Rules’ are designed to help firms apply the FCA’s expectations and build an approach to AI that is both compliant and constructive.
Surprisingly, AI has been in use for some time; however its current, significantly more-advanced form which we’re getting familiar with, demonstrates impressive capabilities to the casual user. Corporates, including insurance firms, are already using it to improve operational efficiency, cleverly create new insurance solutions (Hiscox and Ki) and to enhance customer outcomes.
But, as with any shiny new technology, there are risks. We are still in the early days of AI and much remains unknown. Currently, UK regulators, including the FCA, have not issued AI-specific rules. The FCA is technology-neutral whilst recognising that AI can improve customer experiences and outcomes, but it must be:
“… used safely and responsibly in UK financial markets. […] On the one hand, at the FCA we recognise that firms need regulatory clarity on AI – a predictable framework to guide their investments, operations, and risk management.
On the other hand, we also recognise that if we, as the UK’s financial services regulator, move too quickly or narrowly, we could unintentionally stifle innovation. Also, any regulatory action could potentially become out-dated very quickly as the technology evolves at pace. ”[1].
The FCA has developed a live testing environment to “build trust, reduce risk, and accelerate safe and responsible innovation”, allowing firms to test innovations and engage with the regulator in a consultative manner.
However, for now, the market bears a degree of responsibility for self-regulation, ensuring that AI is used safely and responsibly. With that in mind, here are some suggested Ground Rules for firms experimenting with AI.
[1] https://www.fca.org.uk/news/blogs/ai-live-testing-use-ai-uk-financial-markets-promise-practice

- Include AI in your risk register and relevant policies, with detail proportionate to its use. For example, employees using AI to improve communications should not input customer data into widely-used applications like ChatGPT.
- Maintain a clear ‘Use of AI’ document accessible to employees, so they know what is and isn’t permitted.
- Assign a new operational responsibility for AI oversight to an Approved Senior Manager and update their Statement of Responsibilities. Regulators will ask who has ultimate responsibility within the firm if issues arise.
- Most importantly, if the use of AI determines the outcome of services provided, ensure you have good management information (MI) to allow you to monitor these outcomes and assess whether the outcomes are as expected or if there are any outliers.


- AI can reflect unconscious bias, as it learns from human input. Review MI for unintended/unexpected outcomes.
- Consider AI’s interaction with vulnerable customers. Will it deliver fair outcomes? Can it identify and appropriately support vulnerable individuals?

- AI could have enormous benefits for businesses; however, human oversight is still critical.
- Humans should analyse risks, outcomes, and MI; AI cannot be held solely accountable.
- Ensure you have people with the appropriate level skill and capability to manage AI systems.
- Plan for potential AI failures. Staff should be able to continue operations manually if needed.

- Remember: even without AI-specific regulation, firms must adhere to existing rules, e.g., GDPR and ICOBS. Ensure communications, risk warnings and privacy notices remain up to date.
- Consider whether you meet the criteria to enter into the FCA’s AI Lab and Supercharged Sandbox.
- For firms interacting with or connected to EU entities, note the EU Artificial Intelligence Act (AI Act), effective August 2024. It established a common regulatory framework, classifies AI by risk, and requires transparency. Oversight of the EU AI Act will be shared between national authorities in each member state and a new European AI Office within the European Commission. If an application is categorised as ‘General purpose AI’ (such as ChatGPT), it will be subject to transparency requirements, and those categorised as ‘High-risk’ must meet strict transparency, safety and oversight requirements, and be monitored throughout their lifecycle.
The use of AI will continue to grow. If your firm is considering adoption, proceed with eyes and ears wide-open, balancing innovation with caution.
UKGI, as always, is on-hand to provide guidance and support, so do please get in touch if you have any queries on this topic.

Health Plan 360
A Modern Cash Plan for Today’s Workforce.
Mark Till, CEO, Unum UK
Unum’s entry into the health cash plan space was a logical evolution. Since launching Help@hand, the health and wellbeing app in 2019, we’ve supported thousands of employees with remote GPs, mental health support, physiotherapy and more. But we also uncovered a critical insight: whilst health cash plans are widely available, they’re often misunderstood and underused.
In fact, our research[1] found that:
- 73% of employees had limited understanding of what a health cash plan is
- 17% of employers weren’t sure if they offered one
- 11% of employers have been with the same cash plan provider for six to ten years
This disconnect revealed a clear opportunity: to create a health cash plan that’s intuitive, relevant, and aligned with how people actually manage their health in the modern working world. Health Plan 360 is Unum’s answer – an innovative product designed to simplify access, encourage engagement and support prevention.
[1] Original quantitative research of 500 employees across UK workplaces was conducted from 9th – 16th August 2024 by Yonder Data Solutions.

The UK’s health system is under immense pressure. According to the Office for National Statistics, over 148 million days were lost through sickness absence in 2024. In 2024 alone, our research discovered that one in three employees – the equivalent of 10 million people – experienced a mental health issue, with a quarter reporting that their mental health had worsened. The economic cost of poor health in the workplace is estimated to exceed £100 billion annually, driven by lost productivity, presenteeism and long-term absence.
At the same time, there’s growing recognition that preventative health is not just a personal priority, it’s a business imperative. Chronic conditions such as diabetes and cardiovascular disease are on the rise, linked to lifestyle factors such as obesity, poor nutrition and a lack of physical activity. In response, employers are increasingly shifting their focus from reactive treatment to proactive wellbeing strategies – supporting staff to stay healthy, access care earlier and avoid long-term absence altogether.
Consider this: an average of 4.1 sick days could be saved if employees had access to a health cash plan. That’s not just a productivity gain – it’s also a wellbeing win. It means fewer delays in accessing care, less financial stress and a greater likelihood of early intervention.
Health Plan 360 is designed to meet this need. It’s not just about reimbursing costs – it’s about empowering individuals to take control of their health journey.
Here’s how Health Plan 360 stands apart:
- Digital-first experience: Employees access all benefits through the Help@hand app, streamlining everything from dental reimbursements to mental health support.
- Healthcare navigation: Our navigators guide users to the right care at the right time, saving time and confusion.
- Connected care: A personalised wellness experience that connects all aspects of health, linking services and sharing clinical notes.
- Everyday relevance: From optical and dental to physiotherapy and nutrition consultations, the plan offers fully integrated employee health support that reflects real-world needs.
Health Plan 360 complements and strengthens Unum’s group protection products, enabling a more joined-up approach to care – from prevention to treatment to recovery. For employers it’s a tangible way to show they care while also addressing key business risks like absenteeism and presenteeism. HR managers benefit from consolidated reporting and simplified administration, while employees enjoy a seamless experience that enables them to live a life that is both healthy and happy.
We believe the future of workplace health lies in integration and prevention. Health Plan 360 is our contribution to that future – a smarter, simpler way to support everyday health.
With nearly 3 million people already protected by Unum,[2] we’re proud to bring this new solution to market. More than just a new product, it’s a strategic business asset designed to help people live healthier lives and, in turn, empower businesses to thrive.
[2] Unum internal data as at end of April 2025. Figure represents the total number of lives under all policies and includes the total number of policies for an individual employee where they are insured under more than one product.

