Issue 7 | January 2024


Hello
And welcome.
Dave Middleton, Executive Chair, amii
Welcome to the latest amii members’ newsletter and a belated Happy New Year to you all. I hope that 2024 is a happy, healthy and successful one for you, your families, friends and colleagues.
For those of you who came to the summit in November, I hope that you enjoyed it. The feedback has been excellent, and the turnout of c230 was, I believe, our best ever. There are a number of slides from the event saved on the website in the for Members Only area which are certainly worth looking at, especially the ones around neurodiversity and resilience.
This newsletter includes excellent articles from Bupa about neurodiversity and details on their initiatives to support neurodiversity in the workplace, an introduction to GAIN, of whom we are now corporate members and an article on addiction from our newest corporate members, imatta. If you haven’t already listened to my podcast with ex-professional cricketer Simon Cusden, please log in via Apple or Spotify as Simon opens up about his challenges with addiction, which is fascinating to listen to. We also have an article from Aviva about men’s health and the lack of awareness about testicular cancer, supported by a useful downloadable guide to men’s cancers. This links quite nicely with the webinar we have planned on the 6th of February with HCA on Men’s health – top tips for better health and wellbeing. You can reserve your place via our website events page here.
In other news, we have been looking into whether to have a dinner and entertainment after our Autumn Health & Wellbeing Summit in November and will be sending out a short survey soon to canvas your opinion.
There are a few positions on the Executive Committee that are coming up for re-election, if you are interested in putting your name forward please let me or Tina know before the end of March.
Last but certainly not least I am delighted to announce that we have appointed new compliance consultants UKGI.
UKGI is a market-leading compliance solutions provider for the UK’s insurance industry, and they specialise in delivering engaging consultancy and training services. They are very much looking to build proactive relationships with our membership and will be offering several additional member benefits such as access to templates and toolkits for common compliance questions.
I would like to take this opportunity to thank Branko Bjelobaba of Branko Ltd who has provided the compliance service to our members since insurance regulation began and wish him well as we start on the journey with UKGI as our compliance partner.
We welcome Richard McKenzie, CEO at UKGI, and his team, and I know he is looking forward to working with our members and meeting as many of you as possible at the Spring Summit, where we will be launching a new PMI comparison tool, Claire Ginnelly, Vice Chair, explains more in her article.
Newsletter Contents.
amii podcast
Dr Jamie Barsky, Clinical Psychologist

An introduction to GAIN.
In 2023, amii took the decision to join the Group for Autism, Insurance, Investment and Neurodiversity (GAIN) as a corporate member along with many other insurers and like-minded associations such as BIBA.
GAIN is a community interest company seeking to champion neurodiversity and promote inclusion in the insurance, investment, and financial services industry. They believe embracing neurodiversity – such as conditions like autism, ADHD, and dyslexia – can benefit both individuals and companies.
Led by industry figures with lived experience of neurodiversity, GAIN wants to open up employment pathways for neurodiverse people whose different perspectives and skills are often valuable. They also aim to help companies access this untapped talent to improve decision-making, execution, and business outcomes.
Ultimately, GAIN hopes to facilitate connections that enrich workplaces and positively impact lives. They promote acceptance of neurological differences and self-advocacy to enact positive societal change through diversity of thought.
Over the coming year, you will hear more from us on our progress in working with GAIN and how the benefit of being a GAIN corporate member adds to your amii membership. To find out more about GAIN you can visit their website using this link.
Have you registered to join the for Members Only section of our website?
The for Members Only section of our site provides a wealth of content for members, as well as access to all the benefits that being a member of amii provides. If you haven’t done so already, please do register to take advantage of everything your membership offers. You can do so by following the link below.

Why business
Should be thinking differently about neurodiversity.

And there are specific benefits to building neurodiverse teams. Dr Naomi Humber (pictured), a clinical psychologist and head of mental wellbeing at Bupa, explains, “Having a varied team which includes people who are neurodiverse means that an organisation’s workforce better reflects the demographic of their customer base.[2]
However, recent research reveals an urgent need for greater awareness of neurodiversity, with a 175% increase in Google searches for ‘neurodiverse meaning, a 125% jump in people using the search term ‘types of neurodiversity’ and an 83% increase in Google searches for ‘neurodivergent’.[3]
Judith Singer, the Australian sociologist who is credited with coining the term more than 20 years ago, argued, “We are all neurodiverse, because no two humans on the planet are exactly alike.”[4][5] But today we know it as an umbrella term to describe a range of different ways of learning, thinking and behaving.
Dr Humber says, “We have different conditions that are common when we talk about neurodiversity.[6]
“There is autism, which affects communication, social interaction and behaviour. Attention deficit hyperactivity disorder [ADHD] which affects executive functions such as attention and concentration, and behaviour such as impulsivity. Dyspraxia, which is about physical coordination and difficulties there. And there is dyslexia, which is about difficulty reading and interpreting words, symbols and letters.”
In the past, these differences have often been seen as negatives, but there is growing awareness that neurodivergent individuals can offer sought-after skills including hyper-focus, strong visual, analytical and problem-solving skills, the ability to multi-task and enhanced memory and observational skills.[7]
Dr Humber says, “People who are neurodiverse bring a lot to an organisation and they’re a real asset to the business. They can have impressive attention to detail, amazing energy levels, real focus in terms of certain tasks that they perform. Neurodiversity is sometimes associated with fantastic creativity and the ability to drive innovation by seeing things from a different perspective, and thinking outside the box.”
Seeking out and supporting individuals who are neurodiverse will also become increasingly important in the challenge to recruit and retain top talent.

Central to the Bupa Neurodiversity Benefit is an expert assessment which covers a range of neurodiverse conditions including autism spectrum disorder (ASD), ADHD, dyslexia, dycalculia (difficulty understanding numbers) and dysgraphia (difficulty with writing). It’s important to start with this broad view as these different ways of thinking and processing information often overlap and each person who is neurodiverse is unique.
The Benefit — which is available to businesses with 50+ registrations with packages that include mental health benefits with a minimum outpatient allowance of £1,500 per named employee — also extends to children and dependants over the age of six.
This provides an important pathway to diagnosis and accessing additional support at a time when the average wait time for assessment is almost 10 months,[8] but sometimes extends into years. A report by the British Medical Association found delays of more than two years in England and over five years in Scotland.[9]
The BMA warns, “The potential impacts of a delayed diagnosis on a child’s development are alarming and conversely the benefits of an early diagnosis are wide-ranging.” And the report points out that this can impact the whole family. “A delayed diagnosis denies a child or young person the opportunity to understand the factors that are causing them to respond in a specific way. For families this can create undue stress, with their child’s response to the world often misinterpreted as poor behavioural issues.”
Diagnosis times can also vary in different parts of the UK and Tim Nicholls, Head of Influencing and Research at the National Autistic Society, says, “There is currently a postcode lottery for services, and poorly commissioned pathways for autism assessments which makes it even harder to get the early support that makes such difference.”[10]
However, to access the Bupa Neurodiversity Benefit there is a simple three-step process: clinical triage, followed by a psychiatric and developmental assessment and then a detailed diagnostic report that will include further recommendations and signposting.
First, an employee or their dependant is referred by a GP or, if they are aged between 6 and 15, a special educational needs coordinator (SENCo). If needed, Bupa will pre-authorise their assessment and let the employee know who will be providing the assessment. The employee can then contact the provider directly and arrange an initial consultation at a time that suits them.
If a full assessment is needed, it will be carried out in accordance with best practice within a multi-disciplinary team. This provides the specialist expertise to assess robustly whether someone has a neurodiverse diagnosis or not. The provider will then arrange a follow-up appointment and once this has been carried out, they will produce a detailed diagnostic report for the employee or dependant.

Crucially, if a diagnosis is given, employees are not left in the dark. Bupa will be there to guide them to evidence-based information and resources and ensure they have access to the right support.
And this can take myriad forms. Dr Humber says, “It’s important to get to know the individual and understand their challenges, their strengths, their skills, their uniqueness.
“Communicating is really important. So understanding how you are communicating with people, whether that’s written, verbal or or visual forms of communication. Think about the phrasing you’re using when you discuss things. For instance, if someone is being sarcastic, or uses hypothetical scenarios or metaphors, people with autism might struggle to understand because they tend to be very literal.
“People with ADHD will struggle if you are describing something in great detail that’s quite complex over a period of time. So you might want to give them some written instructions that they can take away and refer back to, if needed.”
Small adjustments to work patterns and ways of working can also make a huge difference. For example, someone with autism may prefer to do the same task on repeated basis, while someone with ADHD is more likely to thrive when offered a range of different tasks and roles.
Dr Humber says, “Open plan offices are often an issue for neurodiverse individuals because they can be an assault on our senses, with bright lights, hustle and bustle, hot-desking, There are a lot of things that go on in a busy office which can make it difficult for someone who is neurodiverse to be productive and successful.”
Think about whether lighting can be adjusted, whether you can provide desk lamps, or standing desks if they want to be a bit more energetic. Noise cancelling headphones, quiet zones and having a dedicated desk or work space can all help to reduce anxiety.
There’s also a growing array of supportive equipment and technology such as speech-to-text and text-to-speech tools, daily planners and mind-mapping software which can be useful.
However, there is no denying that stigma around neurodiversity is still an issue and research from the Institute of Leadership & Management points to some of the barriers forward-thinking employers need to address in order to reap a neurodiversity dividend.
It found that only one in four people would be comfortable recruiting and line-managing someone who is neurodivergent. And looking at specific neurodivergent traits, 69% of diagnosed dyspraxics, 60% of diagnosed autistics and 53% of dyscalculics, felt that colleagues behaved in ways that excluded them, yet only 28% of neurotypicals believed this to be true.
Dr Humber says, “That’s why it’s also essential to promote awareness and understanding in the workplace, and embed an empathetic and person-led culture that supports and champions neurodiversity.”
For more information about Bupa’s Neurodiversity Benefit, as well as some marketing material to support your client conversations, take a look here.
[1] Neurodiversity in Business (NiB): 2022. British Dyslexia Association.
[2] https://www.youtube.com/watch?v=bt83glnULiw
[3] Google search data taken from January – December 2021. Based on internal analysis by Bupa
[4] https://neurodiversity2.blogspot.com/p/what.html
[5] https://neurodiversityinbusiness.org/understanding-neurodiversity/
[6] https://www.youtube.com/watch?v=bt83glnULiw
[7] Workplace Neurodiversity: The Power of Difference part 2; Perceptions About Neurodivergents
[8] Royal College of Psychiatrists
[9] https://www.bma.org.uk/media/2056/autism-briefing.pdf
[10] https://www.autism.org.uk/what-we-do/news/our-response-to-autism-assessment-criteria-changes
[11] Workplace Neurodiversity: The Power of Difference part 2; Lived Experiences of Neurodivergents

Take a listen
The Health and Wellbeing Podcast.
In the latest episode of our popular podcast series, we dive deep into the topic of high performance and addiction. Dave is joined by Simon Cusden, a former professional cricketer, who bravely opens up about his personal struggles with addiction.

Simon shares the challenges he faced growing up, which likely contributed to his struggles with addiction. His battle with addiction began while in Australia for 12 years, involving a suicide attempt and alcohol dependency.
After seeking help from the Player Cricketers Association (PCA) Simon is now seven years sober. He has returned to the UK and started freelancing, focusing on assisting high-performing individuals in senior leadership. Simon offers private coaching sessions and conducts webinars to share his personal experiences and insights.
In the podcast, Simon highlights the importance of recognising and nurturing various aspects of our lives that contribute to overall wellbeing, including mental, emotional, physical, spiritual, relational, financial, and environmental dimensions.
Reflecting on his experience, Simon Cusden shares: “I’ve learned that the most important thing is self-reflection and know that addiction isn’t a problem. Instead, it’s only a solution to a problem.”
We invite everyone to listen to Simon’s inspiring journey and the insightful discussion with him. It is an opportunity to gain valuable knowledge and find inspiration for personal and professional growth.

Addiction, Recovery and
Modern Approaches to Psychological Therapy.
Dr Jamie Barsky, Clinical Psychologist
Lead clinical psychologist Jamie Barsky has completed over 10,000 hours of digital Psychological treatment. He specialises in addiction treatment and recovery and leads the digital treatment pathways of our member organisation imatta. Below he shares expert insight into addiction, recovery and a modern approach to psychological therapy.
I have had many clients ask me how psychological therapy can help them break free from addiction. It can seem pretty unbelievable that ‘talking’ to someone could be a part of the recovery process.
To start to answer this question it is important to first understand what addiction is. Obviously, it is a pattern of repetitive harmful behaviour, which people struggle to resist despite all of the pain and suffering it causes. There are, of course, substances such as alcohol, tobacco and certain drugs which have chemical qualities that cause physical dependence. But, addiction is typically driven by much more than biological dependency caused by the substances. Seeing the harm and suffering caused by gambling addiction, a behaviour which in itself does not cause physical dependence, shows us that it does not need to be an addiction to a substance that can ruin lives.
Psychologists recognise two of the most common psychological pathways into addiction. The most typical route in occurs when a combination of cultural and societal norms and pressures combine with personality and psychological factors. For instance, living in a society or culture in which certain patterns of consumption or behaviour are typical makes it much more likely that individuals within those environments will follow the same patterns of behaviour. If those individuals then have certain personality characteristics, such as high levels of sensation seeking and openness to new experiences, addictive patterns of behaviour become even more likely.
The second most common route into addiction is what might be considered a ‘self-medicating’ pathway. Research shows that people with a history of psychological trauma, mental health difficulties and intense emotions that are hard to manage, are more likely to engage in addictive patterns of behaviour and consumption. Whether it be substance use or behavioural addiction (such as through gambling, sex or gaming), the neurological and physical effects of these addiction behaviours bring short-term relief from psychological suffering. This drives longer standing patterns of these behaviours that cause further suffering to the individual and their loved ones.
Now that we have a basic understanding of some of the routes into addictive behaviours, let’s think about how psychological therapy could be helpful.
Firstly, let me say that it is unlikely that any course of psychological therapy will be exactly the same. Good therapy will always be unique, because a client’s situation is unique. Even with similar types of emotional struggles, people are unique, live in a different context and there are probably big differences that keep them stuck.
That’s why therapy should never be a ‘one size fits all’ approach – experienced clinicians must try to understand their client’s unique circumstances, and to use this understanding to help them with their journey of recovery.
To begin with, the first one or two sessions are spent trying to understand how the problems have developed. This is key. Nothing can be fixed until we know why it isn’t working.
So, bearing in mind that no two courses of therapy will be the same, let me try to offer some understanding of how therapy can help with addiction struggles. Here are some of the key ingredients that might feature in good therapy:
Education – Acquiring new information and knowledge can be empowering. For example, learning about how our brain works can shed light on to why we get caught in unhelpful patterns of thinking and behaviour. This knowledge can help us to override some of the mind traps that keep us stuck in the same patterns of difficulty.
Motivation – Having someone to talk to each week can help us keep focussed on our goals and motivated towards change.
Self-Reflection – Having time to think and talk about our own thoughts, feeling and behaviours can help to understand things in a different way, which can lead to opportunities for behaviour change.
Expressing Emotion – Many people try to ignore painful or unpleasant feelings, thinking they can avoid or reduce them by burying them from their consciousness. Believe it or not, there is loads of evidence to show that bringing attention and understanding to our emotions, and putting our feelings into words, helps significantly to reduce the intensity of them, and helps create new emotional experiences.
Learning Skills – Therapy can be a place where new skills are learnt. Skills for managing emotions, skills for communicating to others, and skills for problem solving can all be important in recovery from addiction.
Seeing beyond the behaviour – Good therapy should look beyond the problem behaviours or symptoms, to understand what might be driving them. Many people with addiction struggles recognise that certain behaviours are a symptom of other problems. Psychologists call this the ‘function’ of the behaviour. What function (i.e. purpose) does the problem serve? This will be a question that most clinicians will ask you to consider and support you to think about.
Remember, as everyone is different, so will be all courses of therapy. Not all of the above elements of good therapy might feature in sessions, but some will and many might.
Modern, digital treatment pathways for addiction have gained popularity and demonstrated effectiveness due to their ability to address key challenges in traditional addiction treatment models. One significant advantage lies in the accessibility and convenience offered by digital platforms.
Individuals struggling with addiction can access support and resources from the comfort of their homes and via a smart phone or laptop. Eliminating barriers such as geographical distance and transportation issues, and better allowing discretion and anonymity.
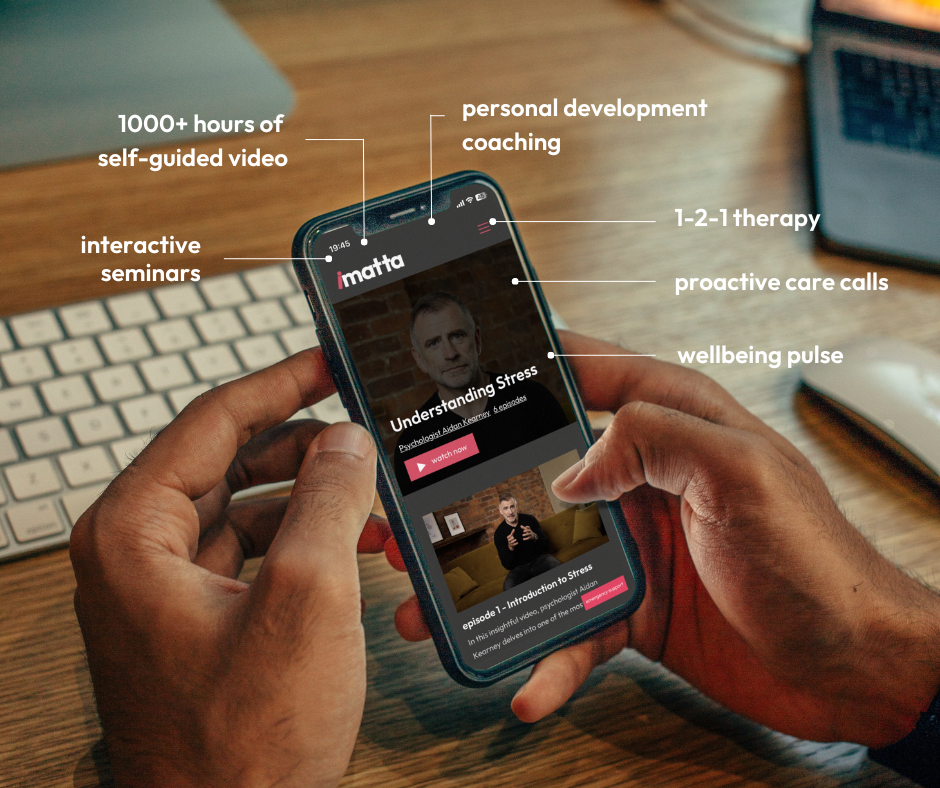
Imatta’s progressive digital wellbeing platform integrates cognitive-behavioral therapy (CBT), mindfulness practices and other empirically supported interventions that encourage earlier engagement and prevention practices.
The interactive and engaging nature of the more holistic digital tools enhances the delivery of therapeutic content, making it more engaging and relatable for users.
amii members offer
Imatta platform that offers holistic mental health and wellbeing support, amii members can get more information by contacting Russel Upton – russell@imatta.com / +44 (0)7944076849
This convenience promotes better engagement, as users can seamlessly integrate treatment into their daily lives without the need for frequent in-person visits. The combination of diverse solutions that encompass various treatment styles and intensities, such as interactive seminars, 1-2-1 video treatment, care calls and wellbeing measurement tools, offer a more holistic and effective approach to addiction recovery as well as general good health and wellbeing practice.
I hope this article has provided some further insight into addiction and the therapeutic treatment and support options available. Please don’t hesitate to reach out to me via the imatta platform if you have any requirements for support, or Russel Upton if you’d like further information on imatta.
Aviva research shows
Worrying lack of awareness of testicular cancer.

Testicular cancer is the most common type of cancer to affect men between the ages of 15 and 49. [1] However, Aviva’s recent research reveals that over a quarter (28%) of men never check their testicles. While 28% said they check their testicles monthly, around one in ten (12%) men said they didn’t think that there were any warning signs of testicular cancer. This misconception was highest in men aged 35-44 years (20%).
Nearly three in five (57%) men knew what to look out for when checking their testicles. However, over a third (37%) of men said they didn’t know the symptoms of testicular cancer. Over a third (38%) of those who weren’t aware of the symptoms, were aged between 25-34 years which is particularly worrying as the peak rate of testicular cancer occurs between the ages of 30-34 years. 2
When prompted, men were good at recognising the warning signs of testicular cancer, such as a painless swelling or lump in one of their testicles (57%), a change in shape or texture (47%) or a dull ache or sharp pain in the testicle/s or scrotum that may come and go (42%) and a difference in appearance between one testicle and another (40%). Just over a third (36%) of men said that an increase in the firmness of a testicle could be a potential warning sign of cancer and a third (33%) said that a feeling of heaviness in the scrotum could be a sign of testicular cancer.
Commenting on the findings, Dr Doug Wright, Medical Director, Aviva UK Health said: “Although testicular cancer is fairly rare, our research reveals a worrying lack of awareness amongst younger men who are more likely to experience this condition. It was particularly worrying to learn that over a quarter of men don’t ever check their testicles and those who do tend to be from older age groups.
“Testicular cancer cases peak in our early thirties but one in five men around this age didn’t know that there are warning signs to look out for. These include a painless swelling or lump in a testicle, a change in shape or texture of the testicle or a dull ache or pain in the scrotum which may come and go.
“The good news is that if it’s caught early, testicular cancer can be highly treatable. So, it’s important that men know what to look for, and get into the habit of checking their testicles on a regular basis.”

When it comes to looking after their health, just over three in five (64%) men agree3 they try to lead a healthy lifestyle, but they know there’s more they can do. Over a quarter (29%) say they exercise regularly, a similar amount (27%) of men say they eat a balanced diet and watch their weight (25%) to help control their risk of developing cancer and other illnesses.
Around one in five (18%) have reduced the amount of fat they eat, and a quarter have either reduced their alcohol intake (15%) or given up drinking alcohol (10%). Just over one in ten have given up smoking
(14%).
Just over one fifth (21%) of men said they aren’t doing anything to reduce their risk of cancer and other illnesses and six in ten (60%) agree they live life how they want, and hope cancer won’t happen to them.
Dr Doug Wright, Medical Director, Aviva UK Health, continues: “It’s positive to see that men recognise the benefits of leading a healthy lifestyle and some are already taking steps to improve their diet, increase their exercise or cut back on unhealthy habits such as smoking and drinking alcohol. “By adopting a healthy lifestyle and being aware of potentially worrying symptoms, men can take positive action to help them control the risk of becoming seriously unwell.”
To help raise awareness of commons symptoms relating to men’s cancers, Aviva has produced a guide in conjunction with Macmillan Cancer Support, which can be shared with clients.
Download a copy of Aviva’s Guide to cancer in men. You can find a copy of the guide here
References
The research was conducted by Censuswide, among a sample of 2002 18+ nat rep general consumers. The data was collected between 20.10.2023 – 24.10.2023. Censuswide abides by and employs members of the Market Research Society and follows the MRS code of conduct which is based on the ESOMAR principles.
1 Testicular cancer – NHS (www.nhs.uk)
2 Cancer research UK – peak rate of testicular cancer cases.
Our events
Register for our 2024 Health and Wellbeing Summits.

Spring Health & Wellbeing Summit
(inc our AGM)
Wednesday, May 22, 2024
The National Motorcycle Museum, Solihul


New member benefit
Benefit comparison portal launches in the Spring.
Claire Ginnelly, Executive Vice-Chair, amii
Great news for amii members to start 2024 as we will be launching our new benefit comparison portal in the Spring! The amii Executive Committee is constantly looking at ways of demonstrating value for money to members and about eighteen months ago we decided a benefit comparison portal would be a fantastic addition to member benefits.
We conducted extensive research of the market to understand what was available and we are pleased to announce we are working with Tendr. Tendr provides tech solutions to brokers and benefit platforms, and they already work with some amii members supporting their businesses. They have a flexible approach to business allowing their clients to choose the benefits and features they want from an extensive list to ensure they have a tech solution which works for the business. The team at Tendr come from a rich tech background and have experience in working with the regulated insurance industry.
The data for the portal comes from The PMI Handbook, which is in its 32nd year of publication. The PMI Handbook is produced by Craigdallie Publishing and Andrew Green of Craigdallie has been working with Tendr for just over a year. Andrew Green has a strong relationship with the PMI insurers which has contributed to the success of The PMI Handbook over the years.
The portal will allow member firms to conduct comparisons of consumer and SME and PMI products in one easy to navigate system and will carry amii branding. Members will be able to download the comparisons in excel or PDF format. It will be free to all amii members, and we will be launching the portal at our Spring Health & Wellbeing Summit on 22nd May at The National Conference Centre and National Motorcycle Museum in Solihull.
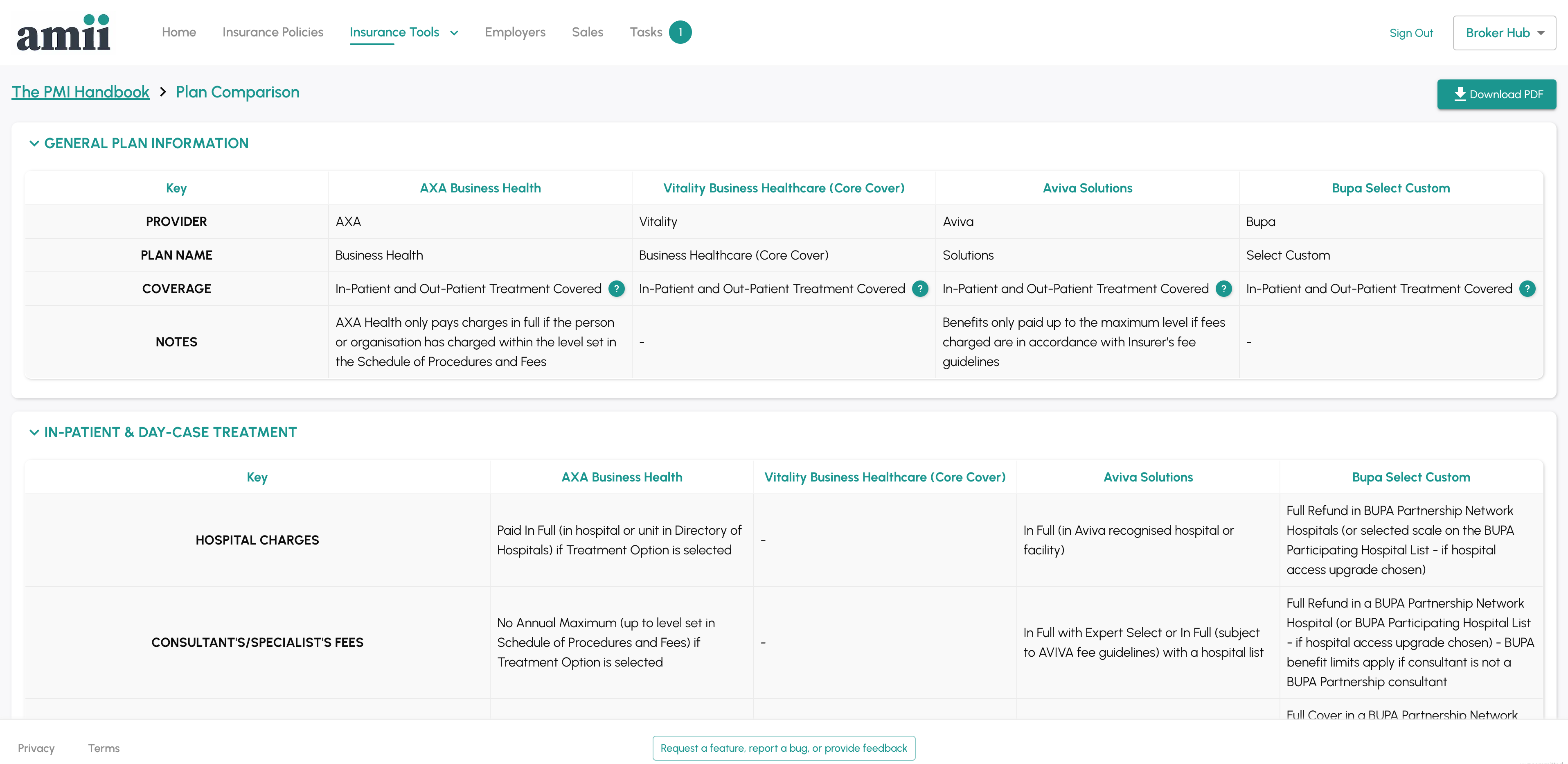
The Executive Committee is very excited about the launch and Dave Middleton, Executive Chair of amii said, “The comparison tool will be a great additional resource for all our members, and we are delighted to have worked with Tendr to provide it. We would also like to thank Paul Nugent from Nugent Santé who helped bring amii and Tendr together.”
Moy Hoque from Tendr said, “We are thrilled to announce our partnership with amii, a collaboration that provides members with a one-of-a-kind benefits comparison tool, fuelled by dependable data from the trusted PMI handbook. Members can now effortlessly compare a wide array of products, covering consumer and SME. Our partnership with amii is part of our wider strategy to provide brokers with essential digital tools to help them improve efficiency, reduce administrative overhead, and enhance the client experience.”
We will be demonstrating the portal at the Spring Health & Wellbeing Summit in May, so we look forward to seeing you there!

